 PREFACE: The following blog was written in a serious tone to convey information in a clear and accurate manner. It seemed reasonable to share my open heart surgery experience - there may come a time when someone that has read the article is faced with a similar situation. Perhaps a word or two will relate to their own recovery and offer encouragement. Just shy of three months since open heart surgery as of this writing and I feel good. My sense of humor has remained intact and there have been fun moments along the way - those moments aren't the focal point of this blog.
I should also mentioned that I stopped using Oyxcodone to manage my pain after two weeks of recovery. There were a couple of reasons for stopping the medication - I'll spare those details in this blog. Another item I neglected to mention is that I chose a natural membrane valve (usually, it's a pig valve) instead of a mechanical valve. As you can imagine, I've heard nearly every pig bacon pork snort sausage joke one could imagine since my pig valve replacement surgery. I'm okay with that ... I can handle it ... as if the jokes couldn't get any worse my own dog "ALF" now refers to me as ... Pig Daddy!!!
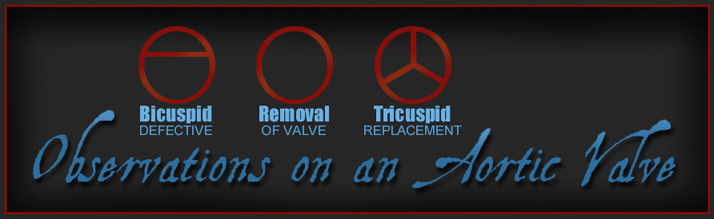
*Bicuspid Aortic Valve Replacement Surgery
During a routine examine in 1991 my family doctor heard a heart murmur through his stethoscope and referred me to a cardiologist to determine the origin of the murmur. An echocardiogram at the cardiologist revealed the source - I was born with a bicuspid aortic heart valve and the separation of the bicuspid flaps was off center which made it even more difficult for the valve to open. A normal aortic heart valve is tricuspid - three fairly symetrical flaps enable efficient blood flow. My cardiologist informed me that valve replacement surgery would be required when I got older. He explained that the natural aging process thickens the bicuspid flaps over time and acceptable heart valve function would deteriorate.
Twenty two years later I underwent open heart surgery at Saint Joseph Hospital on October 14, 2013. My surgeon replaced the defective aortic heart valve and also repaired a hole in my heart. The previous two years had significantly reduced the effectiveness of my faulty valve - forcing my heart to work harder in order to push blood through the nearly closed valve - a process that eventually weakens the heart. On the plus side, a cardiac catheterization performed one week prior to valve replacement surgery confirmed there were no blockages.
Several friends and family members lifted me spiritually and I'm forever grateful for all of their prayers along the way and for their kind words and encouragement. I arrived at the hospital calm and relaxed on the morning of surgery with a 'let's do this thing' attitude. My brother had driven down from Indiana the night before and he followed us to the hospital. My wife and my brother and I were able to visit briefly in pre-op before the nurse began rolling me toward the operating room - that was my last memory until waking up post surgery in the ICU.
The nearly five hour surgery went well. Nurses informed me in pre-op that I would wake up in ICU with a ventilator tube in my throat along with tubes and wires protruding from my chest connected to monitors and other such equipment. Waking up from surgery in the ICU was an unsettling experience - just short of frightening. Waking up on a morphine drip with a ventilator tube down my throat was unpleasant. Verbal communication with my wife, doctors, or nurses was impossible. My wife was allowed to visit me briefly in ICU immediately out of surgery and I desperately wanted to tell her it felt as though I was choking with drainage - attempts at communication were futile.
My wife was allowed back in the room after the vent tube had been removed. I turned my head toward her with a smirk on my face, indicating a less than truthful comment and said, "Maybe they should have let me die." My questionable attempt at humor was to convey my level of discomfort. After several hours the IV was disconnected and oral pain medication was prescribed. Their first choice of oral pain medication didn't work nearly as well as the IV delivered medication. Oxycodone was later prescribed - the dosage, every four hours around the clock. The first twenty-four hours after surgery was fairly painful.
The surgeon and my cardiologist were both pleased with the procedure and expect me to feel better than I have felt in years upon full recovery. While browsing my surgeon's patient notes, collecting papers for insurance purposes, I saw he had written that my diseased aortic valve was one of the worst he had seen. Considering my fairly active lifestyle I feel fortunate that a major heart event hadn't happened before my surgery.
The first two days after surgery were the worst, although each day of recovery had potential for a few surprises. Immediately following open heart surgery your vital signs will be checked every hour on the hour around the clock for the first two to three days and nights. In addition to monitoring your vitals signs, the first week of recovery will focus on pain management, breathing exercises, sitting in a chair, walking down hallways, nourishment, limited leg and arm exercises, and not much else. My cardiologist and my surgeon said my recovery was ahead of schedule according to the time frame. It was several days after surgery before I could express cognitive thoughts on paper due to pain medication, repeatedly drifting to sleep, discomfort, and an occasional sense of helplessness. I had surgery on a Monday morning and was released to come home late Friday afternoon.
Recovering at home - I would suggest scheduling open heart surgery when the temperatures are moderately warm if you have that option. Experience has taught me that cold weather is not a friend to open heart surgery. Dress warm if you must go outside in cold weather and avoid getting chilled if at all possible after such surgery. Your entire body becomes tense when chilled and it puts an additional strain on your healing chest and your incision. It's a momentary discomfort you'll likely notice during your first couple of weeks at home. A serious chill during those first weeks will zap your energy level for several hours and diminish your sense of well-being.
Much of my time was spent sitting in a recliner the first few weeks - this applied to sleeping hours as well as my waking hours. Conventional beds are not comfortable for sleep early on in the recovery process. Around the third week of recovery life became smoother sailing. I began climbing the stairs several times a day and started going for short walks around the neighborhood. After the third week I began dining out a few nights a week and even started going to the movie theater every other week. I took my first post surgery road trip five weeks into recovery. I drove nearly 280 miles that day without incident. Although I was tired by the end of the day ... I felt fine.
Cardiovascular rehabilitation is prescribed to gradually strengthen the weakened heart. The average cardiac rehab program consists of thirty sessions and takes approximately ten weeks to complete based on attending three sessions a week. Providing everything proceeds as planned, during those ten weeks the heart will have been strengthened through a closely monitored and personalized regiment of exercise. I began my cardiac rehab program on November 21, 2013 - three sessions a week. I managed to complete nine sessions before returning to work on December 12, 2013. My intention is to schedule the remaining twenty-one sessions around my work schedule.
Keep in mind that full recovery usually takes at least six months. Granted, six months might seem like a long time given the fact my diseased valve had been replaced with a near perfect valve. The six month time frame was expertly explained to me when I started the cardiac rehab program. During surgery a near perfect valve was placed in my heart and the replacement aortic valve is working properly. The next phase of recovery is far less dramatic and requires much more time. Since my heart had been stressed for so many years due to the faulty valve, the walls of my heart had thickened and my heart had weakened - become less efficient. My heart must now be strengthened ... gradually.
The purpose of this essay is to provide a glimpse of encouragement for anyone that might be anticipating [or recovering from] a similar surgery. Recovery has it's moments - there are bad times and better times, yet recovery is very doable. Mental preparedness is an important aspect of your post surgery transition. Preparing yourself for the occasional obstacle will help you through the challenges of such a life event. I consider these suggestions useful tools that will help combat the negatives.
I mentally prepared myself as best I could before surgery - realizing my life would change significantly for the next two months. Proper use of mind over matter can keep moments of depression in check. Don't kid yourself - you will face some challenges and surprises on your journey toward recovery. You should expect some days to be easier than others. There will be days when you feel as though you've taken two steps backward ... and yet, the next day might feel more like three steps forward. I had made excellent progress entering into my fifth week of recovery - I felt good! I was active once again - the exception being heavy lifting and physical labor - such activities were restricted at that point in recovery.
Never completely take positive progress for granted. I experienced extreme lower back and chest pain and deep breathing became labored late one evening in December. The pain occurred without warning and for no apparent reason. I never imagined the pain had anything to do with my heart since I had been doing extremely well and feeling good for weeks. I couldn't figure out any reason for such pain. I decided the pain must have been the result of a muscle spasm or a pinched nerve - that's what I convinced myself. You might have guessed by now, being the guy that I man ... I didn't call my doctor or go to the emergency room that evening.
When I explained the pain I had experienced the night before to cardiac rehab staff the next day, they asked me numerous questions then explained that I should have sought medical attention. A staff member then called my cardiologist and scheduled me an appointment for the next day. Lesson learned - regardless how many weeks into recovery you are, if you experience significant pain and/or shortness of breath after having heart surgery, call your doctor or go to an emergency room to determine the source of your pain.
I went to the appointment and an echocardiogram determined that a small amount of fluid had gathered around my heart. I was also experiencing some mild inflammation in the region. Based on those findings, chest x-rays and lab work were also scheduled. The chest x-rays and three of the four different blood labs came back fine, however, one lab revealed an elevated number a bit higher than normal so a CT scan was scheduled for December 16th. The CT scan indicated there wasn't a blood clot or anything else wrong and fortunately, that pain and shortness of breath event has been an isolated one time occurance and significant pain medication subsided the symptoms by the next morning.
Doctors and cardiac rehab staff advised against returning to work full time right out of the gate. I returned to work on December 12, 2013 and worked my normal hours for the week. Fortunately, work was fairly slow that week - toward the end of my shift I began noticing some aches and pains. After being off work for two months I never considered how many arm, shoulder and neck movements are unique to the job. After taking a couple of Advil those aches and pains were supressed and I completed my scheduled work week. I ruled my first week back to work a success. I was able to do my work and endure eleven hour work days by properly pacing myself.
I'm grateful for the commitment and expertise of my surgeon Dr. Dermot Halpin, my cardiologist Dr. David Cassidy, and to the nurses and staff at St. Joseph Hospital. To recap the most important aspect of post open heart surgery - expect a few surprises on your journey to full recovery - there will be bumps in the road. My optimism toward full recovery has not diminished. Remain tough and stay focused on your recovery. Hang in there. Keep the faith. Follow medical advice. I'm feeling good and even better days are on the horizon!
Mark McKinley - Lexington, KY - updated April 13, 2014
(C) 2013 mogswebsite.com
*Bicuspid Aortic Valve - A bicuspid aortic valve (BAV) is most commonly a congenital condition of the aortic valve where two of the aortic valvular leaflets fuse during development resulting in a valve that is bicuspid instead of the normal tricuspid configuration. Normally the only cardiac valve that is bicuspid is the mitral valve (bicuspid valve) which is situated between the left atrium and left ventricle. Cardiac valves play a crucial role in ensuring the unidirectional flow of blood from the atrium to the ventricles, or the ventricle to the aorta or pulmonary trunk. Source: Wikipedia
|
Website Design by Mark McKinley
graphics, logos, photos (C) 1999-2022 Mark's Online Graphics Site